
Our lives have been transformed by Covid-19, and in the short term, they will change still yet. But what will happen after this pandemic is over? Will life go back to the way it was? Dr Leonid Shapiro, managing partner at Candesic, looks beyond the immediate crisis gripping health systems to explore the impact the outbreak might have on the NHS and social care in the longer term
It looks like Coronavirus is here to stay, at least until a vaccine is developed in one to two years’ time. So, what does the new world look like and what impact will it have on health and social care in this country?
Before exploring this impact, we should first review the facts about Coronavirus, or more specifically, the Covid-19 variant.
Covid-19 belongs to the same family of virus that cause the common cold. What’s different with Covid-19 is that it uses the ACE2 host receptor to enter cells, and that this receptor is common in airway epithelia and lung parenchyma cells. This means that Covid-19 is particularly good at infecting lung cells deep in the lung. So, unlike the common cold, which typically affects the upper airways and throat, Covid-19 attacks the entire lung and can readily cause bilateral interstitial pneumonia (infection of the entire lung on both sides).
Covid-19 is much worse than the ‘flu’
Covid-19 infections are similar to those of common flu (caused by the influenza virus) in that both more easily move to the lungs than the common cold. When this happens, it can be deadly for those with poor health. Thousands of people die each year from seasonal flu in the UK, so why are we so much more worried about Covid-19?
There are several reasons and they are driven by key differences between flu and Covid-19.
Firstly, Covid-19’s incubation period (the time between infection and showing symptoms) is 2-3x longer than the flu. This means that people who are carriers are out in the general population longer before they know they are sick.
As a result, the R0 (a measure of how many people one infected person infects) for Covid-19 is almost twice as large as for the flu. The result is that it is much more contagious and spreads faster…much faster.
An R0 of 2 means that infections could grow exponentially, 2, 4, 8, 16, 32, 64, infecting pretty much everybody in a short time. Covid-19 R0 is estimated at just under 3.
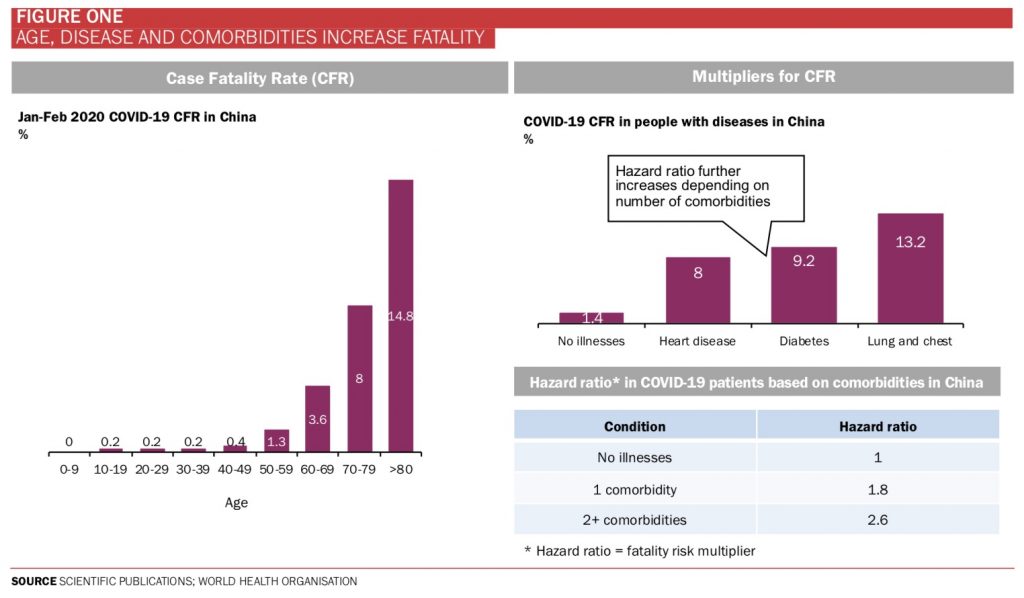
Secondly, the Case Fatality Rate (CFR or ‘death rate’) is between 20-30 times higher. Still not as high as SARS which was 100x higher, but SARS was much less contagious and was therefore able to be contained.
Thirdly, there also is no vaccine for Covid-19 at present. A flu vaccine does exist, but its effectiveness is variable as scientists attempt to guess the likely strains each year and don’t always get it right. In the UK, deaths from the flu range from 1,692 in the winter of 2018/19 (when a good vaccine was available) to 28,330 in 2014/15 (when the vaccine was poor).
The combination of these three differences means that we should sadly expect deaths from Covid-19 to be in orders of magnitude larger than the c.20k flu deaths seen in the UK each year.
The UK fairs pretty well on the global stage
It’s known that Covid-19 can range from being asymptomatic, particularly in children, to being deadly in frail elderly people and those with underlying health conditions. The case fatality rate (CFR) varies dramatically with age and health condition (Figure One).
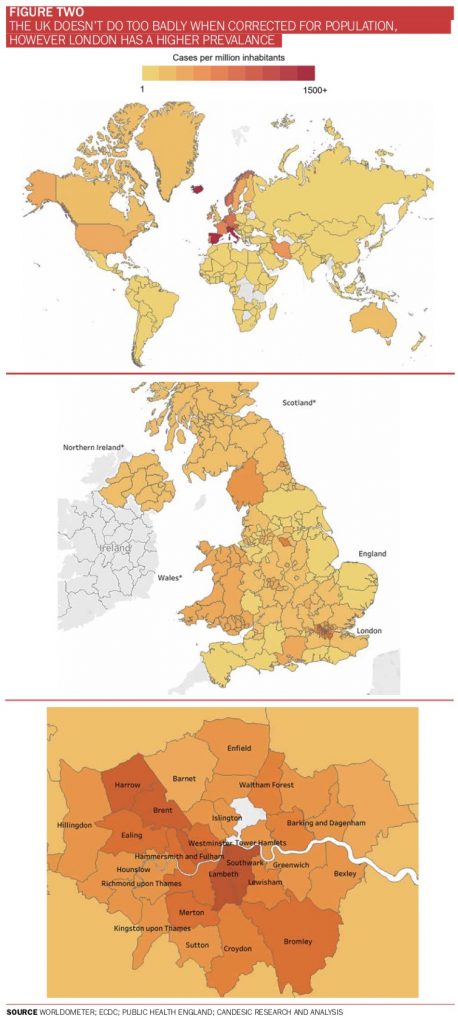
We’ve seen many maps showcasing reported infections per country, but we have analysed the same data based on population.
We see the UK is a relatively safe place to be compared to many other large nations. However, in the UK, London has a higher prevalence, as would be expected due to high population density and international visitors (Figure Two).
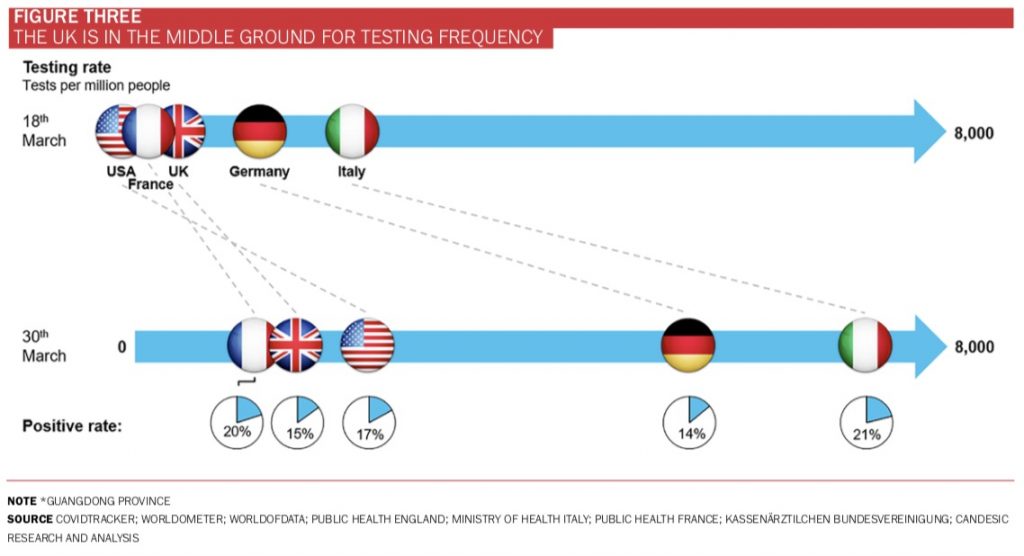
The UK is also doing a fair amount of testing compared with other countries, suggesting that prevalence rates, although likely to underestimate the true level of infection, can be legitimately comparable to other countries, at least on a relative scale (Figure Three).
Despite some countries doing better than others, it’s likely to be only a matter of time until most of the UK population is infected and some academics estimate the eventual infection rate to be c.80%.
The UK has moved from containment stage to delay stage, an acknowledgment that widespread infection is inevitable.
There will be shocks to healthcare, social care and business.
To help prepare, worse-case scenario planning is essential, particularly for providers/businesses who care for elderly frail and/or sick people.
Government will have to bail out care home providers
The very likely spread of Covid-19 to most of the UK population combined with the deadly impact it has on old, frail and sick people has the potential to have a devastating impact on society and in particularly, care homes for older people.
As well as advanced years, care home residents tend to have poorer health than those of the same age living independently. For example, people in care homes have twice as much chance of having long term conditions such as COPD, diabetes, or heart disease (Figure Four).
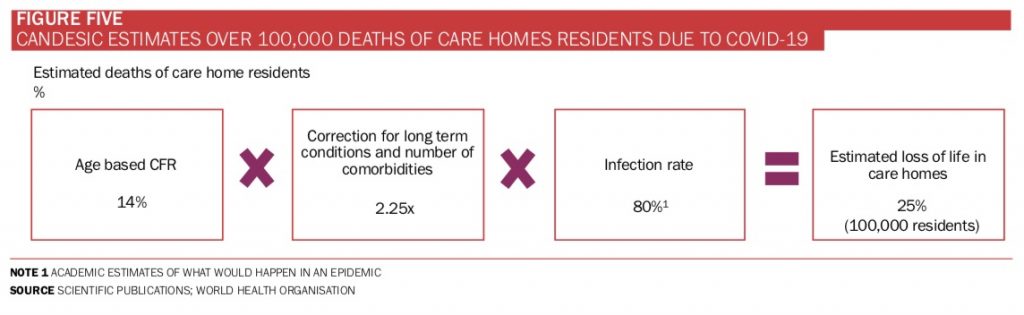
Candesic estimates that if Covid-19 become endemic, we may lose a quarter of the c.400,000 older people currently living in UK care homes.
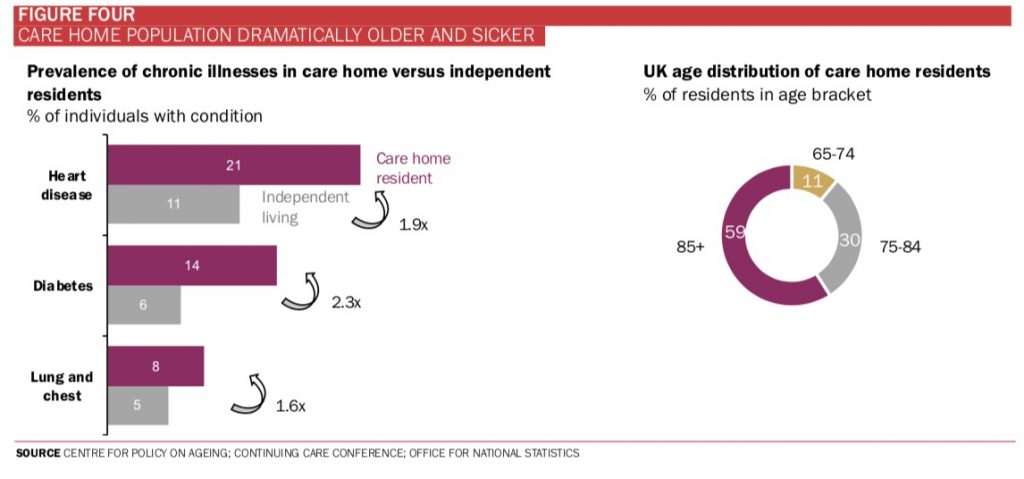
We have estimated this by applying Covid-19 fatality rates by age to the demographic in care homes and correcting this by higher prevalence of poor health and larger number of co-morbidities seen in care homes.
The stark figures reveal that even if only 80% of residents become infected, 100,000 care home residents could die as a result of Covid-19 (Figure Five).
Care home operators are already taking precautions to reduce the chances of Covid-19 taking root in their homes. Many have banned visitors, but the much-needed carers and other staff, many of whom could be infected and asymptomatic, could inadvertently spread the infection.
Solutions such as isolation with permanent/live-in staff are likely to be impractical and unaffordable. Another solution may be to use staff who have already been sick and recovered and may be immune. However, the number of such staff is likely to be low early in the infection cycle and by the time there are enough of them it may be too late.
Even if somehow operators were able to completely shield residents from Covid-19, older people who might be future residents who are currently living on their own will still be affected by Covid-19 and many may not ever make it into a care home.
Many GP surgeries will be permanently closed
We are all aware of the rise of video-based consultation from the likes of Babylon, Push Doctor, Doctor Care Anywhere, Livi and many others.
According to Babylon, c.85% of its video consultations do not need to be followed up by physical ones. This means that in most cases, physical consultations can be avoided.
One could imagine that if penetration of video consultations went to 100% of the population, we could see the demand for physical GP surgeries halve. However, current penetration is just 2%.
GP surgery providers have not been worried because the mainstay of GP visitors, elderly patients, have not adopted video consultations. Elderly patients are twice as likely to visit GPs and, to date, do not materially use video consultations (Figure Six). However, Covid-19 will change all of that.
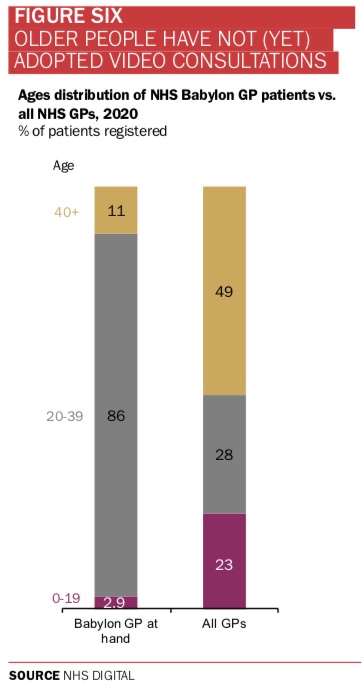
It’s clear that older people, who visit their GP for non-Covid-19 issues often, will more readily adopt video consultations to benefit from reducing their exposure to people with Covid-19 in GP waiting rooms.
This phenomenon is likely to see the largest cohort of GP users, the elderly, replace physical visits with digital solutions, dramatically reducing the need for physical GP surgeries.
Sure, many consultations can’t be effectively done digitally, but enough will be to reduce the need for GP surgery physical property.
After a period of shock, the NHS will have breathing space
At the moment, the NHS is under immediate threat of being overwhelmed by the pandemic, but the tragic irony is that widespread Covid-19 fatalities could dramatically reduce its costs in the medium term.
Healthcare systems around the globe are battling to meet rising demand from an ageing population, a significant proportion of whom are living with long-term health conditions and have multiple morbidities.
The sad fact is that the number of long-term conditions we are likely to suffer increases as we age, and as a result, add significant cost to the NHS (Figure Seven).
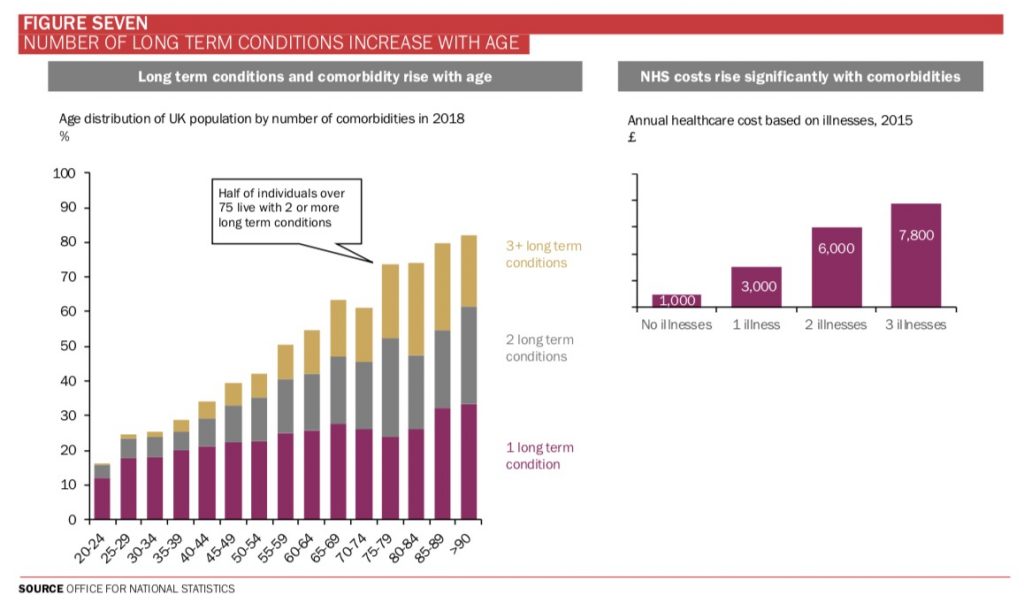
As the population ages, this is the primary driver of the growth in demand and why costs are growing above the rate of population growth alone.
Older people with long term conditions are most at risk with Covid-19 and, as unintended a consequence as it may be, could result in a reduction in NHS costs in the medium term.
It’s well known that a small number of people account for a disproportionately large part of healthcare costs. Candesic analysed the unplanned healthcare costs of the population of Cambridge and Peterborough and found that 15% of the population accounted for almost all unplanned NHS costs (Figure Eight).
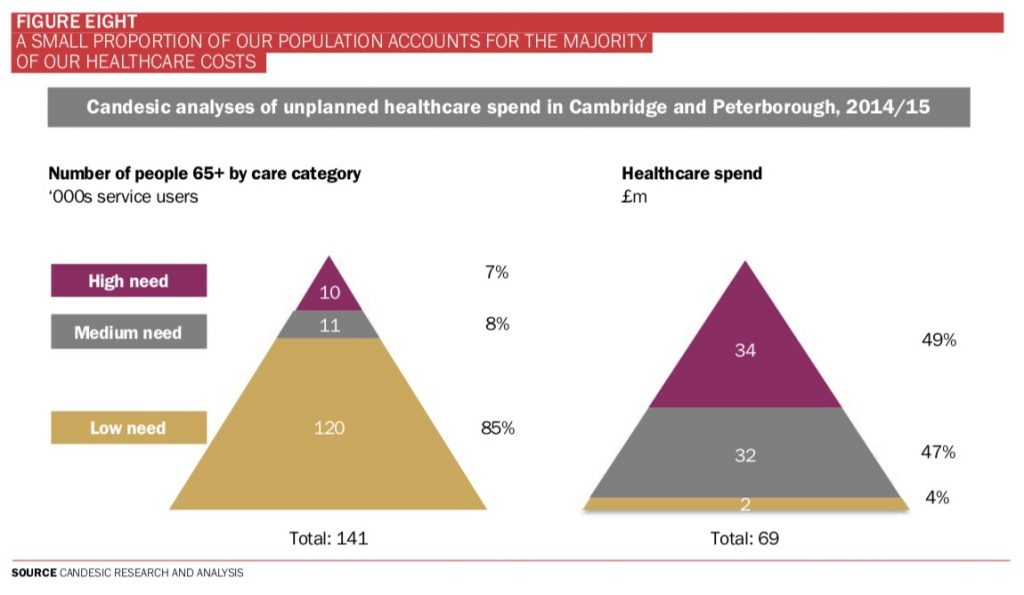
Despite a peak demand in the short term, the NHS could potentially see reduced costs in the medium term as a result of Covid-19.
The long-term effects of Covid-19 are hard to predict, but for sure, it is not the last time we will have a deadly pandemic.
If Covid-19 is brought under control or even eradicated, say with the help of an effective vaccine, our population will quickly redistribute back to the current level of elderly people living with long-term conditions.
We must use this time to find ways to better manage population health, deliver healthcare more cost-efficiently, and innovate to be ‘at the ready’ for the next pandemic.







 ©2024 All rights reserved LaingBuisson
©2024 All rights reserved LaingBuisson 


