 Employee Assistance Programmes are moving beyond the provision of ‘light’ support to become all-encompassing wellbeing programmes. And, with increasing digitalisation and awareness around mental health in the workplace, they have the potential for continued growth, explains Candesic’s Marc Kitten
Employee Assistance Programmes are moving beyond the provision of ‘light’ support to become all-encompassing wellbeing programmes. And, with increasing digitalisation and awareness around mental health in the workplace, they have the potential for continued growth, explains Candesic’s Marc Kitten
While Employee Assistance Programmes (EAP) are not new, there are several forces converging in this age of digitalisation and mental health awareness that are turbocharging the focus by corporates and employees on such programmes. You can call it EAP 2.0.
Several push forces have recently driven an expansion in the scope of services offered under corporate EAP programmes, as well as the number of companies offering them:
- In a historically low unemployment environment across the globe, particularly for younger employees, the increased competition for talent is leading to wellbeing benefits being shaped as a competitive advantage in recruiting. Salaries and titles are no longer enough to attract and retain the best talent. At the same time, providers of EAP services such as insurance and HR management companies push for corporates to adopt such programmes creating a virtuous demand and supply cycle.
- Digital technologies are enabling providers and employers to offer more services at a lower cost and consequently lower price point. Examples of such technologies are self-help apps, whether proprietarily developed or third party, and remote wellbeing consultations (which attracted significant technology investment under Covid).
Reinforcing these push forces, there are equally important and powerful pull forces. Increased attention on wellbeing and mental health is coming from various angles:
- Macro events over the last few years have exacerbated some of the trends that can put increased pressure on wellbeing – these include reduction in social face-to-face interaction due to increased virtual social and work time, ever increasing cost of living with employees continuously losing purchasing power (affecting particularly younger workers) and reduced on-the-job training/lower investment in onboarding due to work-from-home dynamics and overall corporate efficiency drives.
- Younger cohorts of workers are making up an increasing proportion of the workforce and, as opposed to older generations, they are more aware of the importance of staying healthy both physically and mentally. Millennials and Gen Z workers are expected to make up around two thirds of the workforce in Europe by 2025 – almost doubling from around one third ten years ago. Also, their willingness to use company provided digital health services is significantly higher than that of older generations.
The scope of EAP is evolving
The origins of EAP can be traced back to the late 1930s. They began in the US as programmes to deal with occupational alcoholism. Fast forward to today and EAP programmes are not only a relatively standard component of employee benefit programmes, but also include a wide range of support services, covering diverse matters beyond mental health and addiction to areas such as family counselling, general lifestyle, personal finance support, legal counselling and a myriad of specialised advice areas (Figure One).
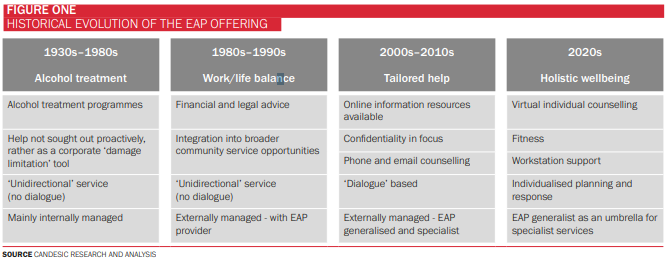
As EAP has evolved to become an all-encompassing employee wellbeing offering, it is increasingly integrated by the large healthcare insurance providers, such as AXA, Bupa and Allianz, into occupational health programmes providing holistic healthcare support to employees. Recognising this trend, programme providers focused exclusively on EAP have sought alliances with fully integrated suppliers, or been acquired by such, to complement and complete the traditional occupational health offerings. Examples include Optima Health’s partnership with Bupa or Optum being acquired by the leading US healthcare insurance provider UnitedHealth.
In general, we should expect to see increased consolidation in this space and in the overall wellbeing sector – whether between direct competitors or between competitors with complementary offerings. The merger between Babylon and MindMaze, which was just announced, emphasised the ability to offer an increased breadth of solutions to their customers, as well as benefits from scale that will allow the combined company to accelerate their investment programmes.
External factors supporting the growth in EAP
The impact of the well-publicised increases in waiting lists across Europe has not escaped the provision of mental care. According to the European Commission, in 2022, about a quarter of adults needing mental health assistance in Europe were not getting the help they needed – with the proportion for younger patients (18-29) being close to 50%. The need for wellbeing and mental health support is as high as it has ever been, and the cases being treated do not appear to be able to keep up with demand for reasons beyond the scope of this article.
Available EAP data comparing performance to public services along various metrics, show that EAP programmes are doing better in terms of efficiency. Shorter waiting time from referral to initial treatment, or to follow-up sessions, and a higher percentage of patients completing treatment, are translating into individuals who have corporate EAPs reducing their reliance on the public sector. Also, EAP mental health services have become more sophisticated and agile over time, and able to offer more breadth of treatment. Coinciding with the integration of EAP into broader corporate healthcare plans, individuals can now be increasingly supported beyond first contact and access full treatment.
However, this shift from what were supposed to be light support and assistance programmes into front-line acute services does have significant impact on how they are, and should be, administered. A transition towards EAP delivering more critical services drives the need to have more specialised personnel to successfully deliver treatment.
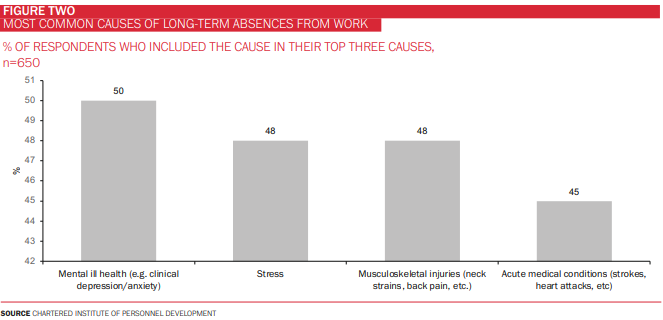
A further factor accelerating the demand for EAP services is driven by the rise in work absenteeism. Over the past three years, in the aftermath of Covid, the trend in absence from work due to long-term illness (both mental and physical) has been of steady growth with anecdotal data showing absences at all-time highs across Europe. Employers are logically leveraging their EAP offerings to engage with employees in addressing the causes of absenteeism. Employees find that the multidisciplinary approach to healthcare of EAP works well for them, given that the reasons for absenteeism are often multiple and complex (Figure Two).
EAP is a win-win for everyone
We expect the prevalence and relevance of EAP to continue to rise given the strong supporting fundamentals. There are numerous cost benefit analysis that show that EAP programmes more than pay for themselves through reduced employee absenteeism, increased employee satisfaction and improved employee retention. There are also numerous surveys that show high employee satisfaction with the EAP programs offered by their employers. We believe these dynamics will continue to reinforce themselves.
However, there continue to be areas of improvement for the sector. A number of current offerings, though there are notable exceptions, are seen as mostly reactive rather than proactive. Recognising that proactive management requires more resources, and is therefore more costly to providers and employers, the very attractive return on investment would suggest there is still room to allocate more resources to further this virtuous circle. The second major area of focus should be around EAP being seen as providing more than a short-term fix by moving more towards the provision of in-depth screening, treatment, care and rehabilitation to employees in need. As mentioned before, the bridge to close the circle with occupational health is already there, and the distinctions between the various healthcare and wellbeing programmes are becoming less clear.
And beyond the strong tailwinds, what is equally promising is that EAP is a clear beneficiary of the increased digitalisation of healthcare services, which translates into improved patient outcomes by doing more with less. Many digital providers are increasing the range of products available, while bringing down costs through the use of technology. Examples include generalist providers such as Liva Healthcare (coaching to manage lifestyle and chronic diseases), Koa Health (personalised and accessible mental health solutions) and Big Health (non-drug alternatives to mental health recovery), as well as specialist providers such as Oto (services to chronic sufferers of tinnitus), Kaia Health (digital health services for musculoskeletal pain) and TuMeke (AI ergonomics assessments for the manufacturing sector).
A final thought on the possibilities that this new era of EAP is bringing is around how public-private-partnerships can develop to leverage expertise, resources and capabilities for the benefit of employees. The public sector has been for many years the main provider of solutions to address mental health related issues and has accumulated vast knowledge on treatment and therapy. Equally, EAP programmes are proving to be an effective first point of call with their broad networks and touchpoints with the labour force. The potential to combine the front-line and triage capabilities of EAP, with the treatment and therapy capabilities of the public services could be explored further.








 ©2024 All rights reserved LaingBuisson
©2024 All rights reserved LaingBuisson 


