In past years, outbound medical tourism from the UK has been driven by patients seeking to save money by travelling for cosmetic surgery and dental treatment in lower cost destinations in Europe, such as Hungary, Poland and Turkey. Has the impact of the pandemic expanded the outbound medical tourism market from the UK?
Prior to the pandemic, many hospitals, clinics and facilitators across Europe saw the UK as a rich source of medical tourists, and despite much of the negative publicity in the UK media, there was a steady growth in the number of patients travelling for lower cost cosmetic surgery and dental treatment, and to some extent for IVF. Estimating the number of such medical tourists has never been easy, despite the efforts of the Office of National Statistics to monitor such activity through the International Passenger Survey. However, the small size of the data sample, makes it difficult to put an accurate figure on the outbound flow. It may be 50,000. It may be 100,000. It may be more, or much less. No-one really knows.
Since the pandemic, destinations are reporting the recovery of medical tourism from the UK. However, inflation, the current recession and the resulting pressure on disposable income may, in fact, restrict the flow of patients for “discretionary” treatments such as cosmetic and dental. But on the other hand, has the pandemic driven demand in other areas of healthcare?
To gauge this new demand, we need to look at how the pandemic has affected UK patients access to health services.
How Covid-19 has impacted UK healthcare
The impact of the pandemic on NHS capacity, the underfunding of public sector healthcare services, and the severe staff shortages (partially as a result of Brexit – the number of new nurse registrations from the EU has dropped by 87%), have meant a steep rise in waiting lists and pent-up demand for healthcare. The main drivers have been and continue to be:
- Patients on waiting lists for NHS treatment who would ordinarily have been seen by now.
- Patients who have not yet presented to their GP (primary care physician) to seek a referral for symptoms due to concerns of burdening the health service or fears around COVID-19 infection.
- Patients who have had operations cancelled due to staff shortages.
- Patients who have had consultant/specialist referrals delayed or cancelled.
- Patients who have had referrals refused due to a lack of capacity.
- Patients who are unable to secure prompt access to primary care services, creating a delay in initial diagnosis and referral.
Prior to the pandemic in February 2020 there were already 4.43 million patients on a waiting list for care in England. The latest figures show:
- A record of 7.1 million people waiting for treatment at the end of September.
- 87 million patients waiting over 18 weeks for treatment.
- 401,537 patients waiting over a year for treatment – which is over 400 times the 1,032 people waiting over a year pre-pandemic in July 2019.
- A median waiting time for treatment of 14 weeks – significantly higher than the pre-COVID duration.
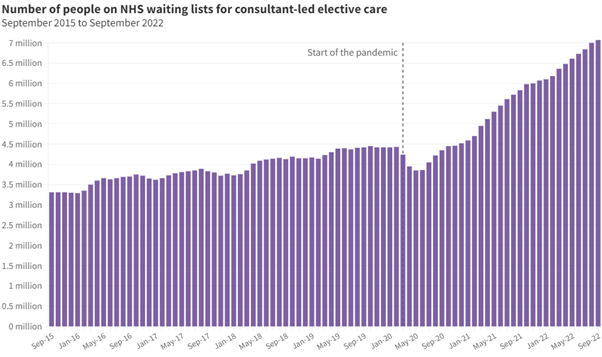
Source: BMA analysis of NHS England Consultant-led Referral to Treatment Waiting Times statistics
All areas of healthcare are being affected, including serious diseases such as cancer and heart disease which in normal times would be seen within a two-week referral target. The Office for Health Improvement and Disparities (OHID) reports that since the beginning of September, there have been nearly 900 more deaths in people with cancer than would be expected at this time of year.
Here is the picture for cancer referrals.
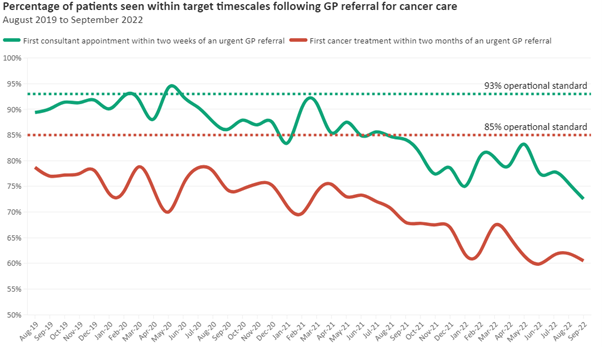
Source: BMA analysis of NHS England Consultant-led Referral to Treatment Waiting Times statistics
The proportion of patients seen by a specialist consultant within two weeks of an urgent GP referral for suspected cancer is extremely low. The 93% target for patients to be seen within the two-week target has not been met since May 2020.
Some efforts have been made to outsource NHS patients for treatment in the UK’s private hospitals. However, there are capacity issues in the private sector due to increased demand in the self-pay market and the backlog of private sector patients.
The growth of self-pay treatment
Self-pay treatment is where a patient who is not covered by health insurance, decides to pay cash (or take out a loan) for treatment in a private hospital under a fixed price surgery package. Typical prices for this from a major UK provider:
- Hip replacement – £12,500 (US$14,800)
- Knee replacement – £12,500
- Cataract surgery – £2,650 (one eye)
According to the Private Healthcare Information Network which gathers data on private healthcare activity, when comparing July to September 2019 and the same period for 2021, there was an increase in self-pay of 35%, with 67,100 people opting to pay out-of-pocket for private treatment. Spire Healthcare reported a ‘sustained switch’ in consumer attitudes towards private hospital care and that private patient revenue was up by more than 30% on pre-pandemic levels. The move to self-pay also extends to those areas where patients would normally expect prompt treatment under the NHS. The monthly number of privately funded chemotherapy sessions reached 13,200 in 2021, up from around 10,000 in February 2019.
So… what is the opportunity for destinations to target the UK?
In the past, few UK patients have chosen to go abroad for major surgery. However, the current state of the UK’s health services may encourage UK patients to expand their horizons in terms of treatments that they seek and the destinations that they may consider.
That represents an opportunity for agencies and facilitators, and hospitals and clinics in lower cost destinations that can reassure UK patients about the quality of care and treatment outcome. If you’re looking at this business opportunity, here are some things to consider:
- Price – how do your prices compare to those within the UK’s private hospitals when the cost of travel and accommodation are factored in?
- Have you considered providing finance/loan arrangements for patients?
- Can you offer an all-inclusive, fixed price package that matches the offering of a UK private hospital?
- Quality – can you provide proof of your standards of care and importantly… outcomes?
- Patient support – how will you support the patient throughout the patient journey, particularly when they return home.
And finally, how will you generate enquiries and attract these UK patients? Make sure you include LaingBuisson’s patient acquisition site, Treatment Abroad in your marketing plans!








 ©2024 All rights reserved LaingBuisson
©2024 All rights reserved LaingBuisson 


